 What is Splenic Flexure Syndrome & How is it Treated?
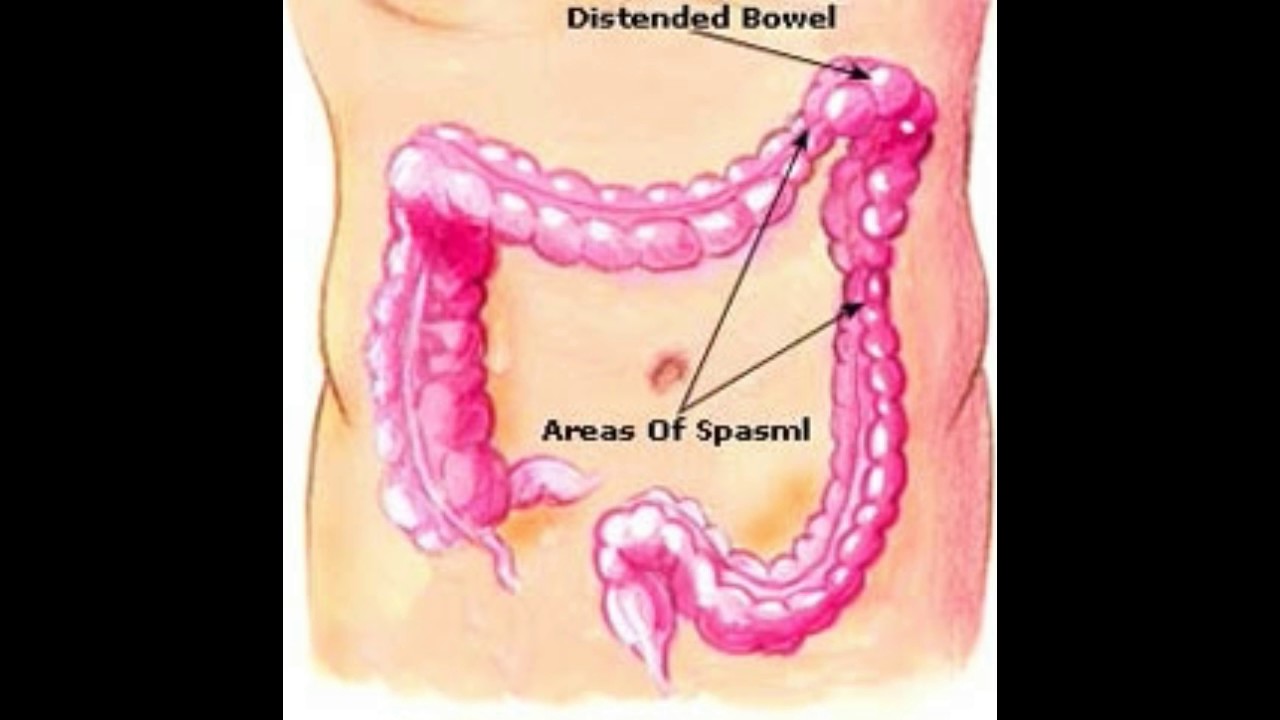
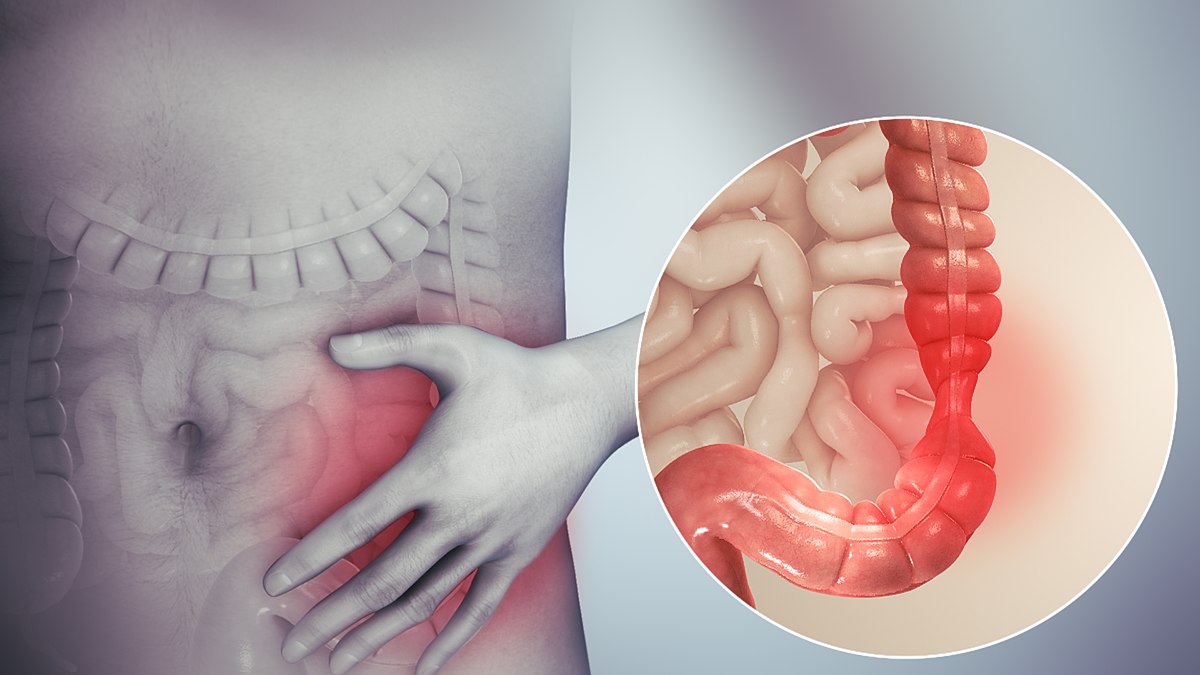
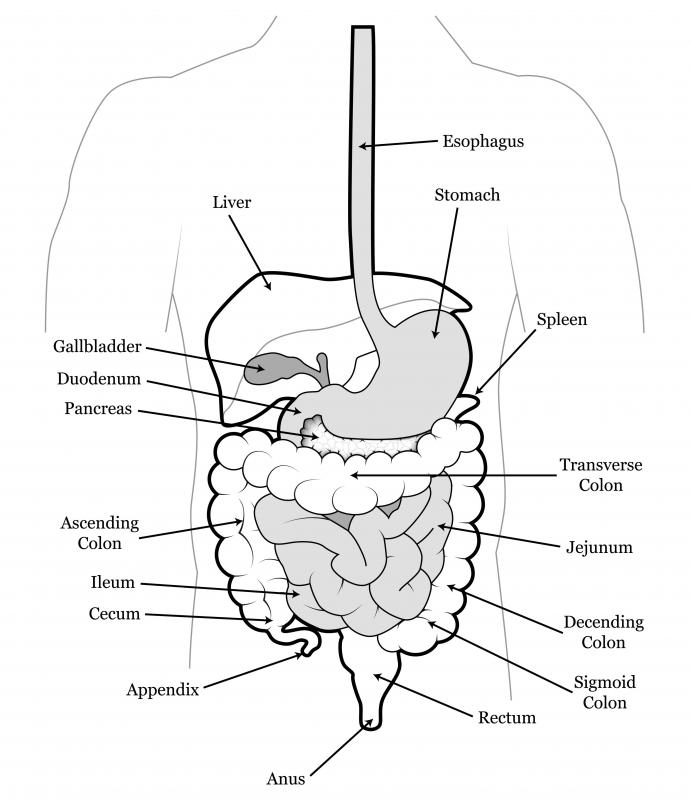
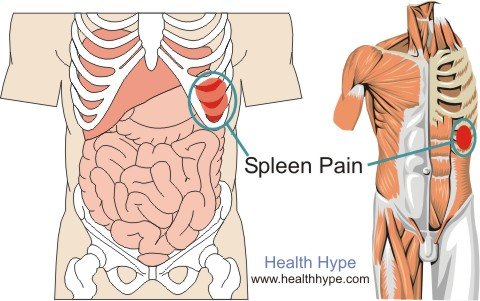
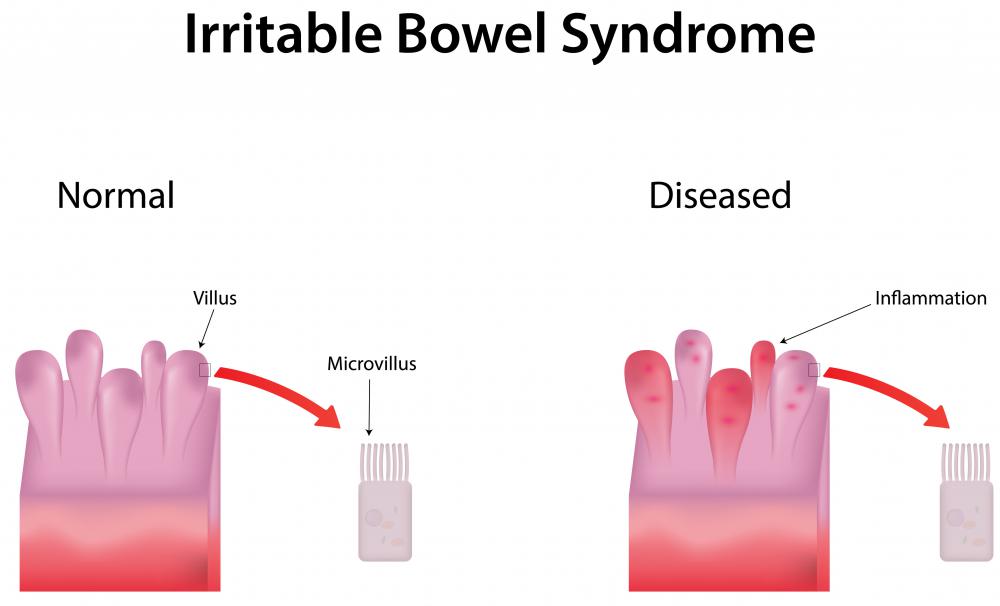
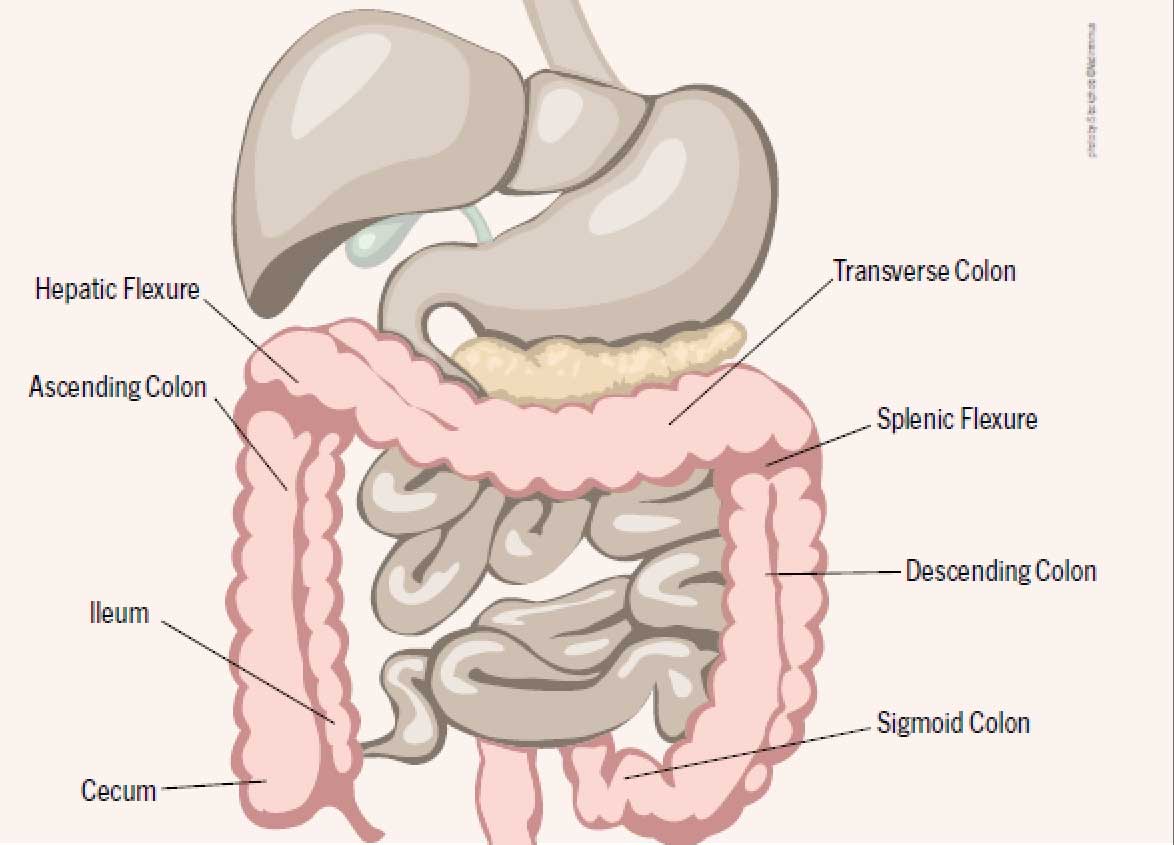
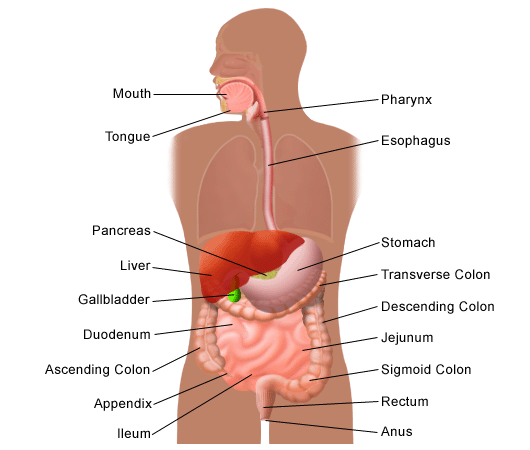
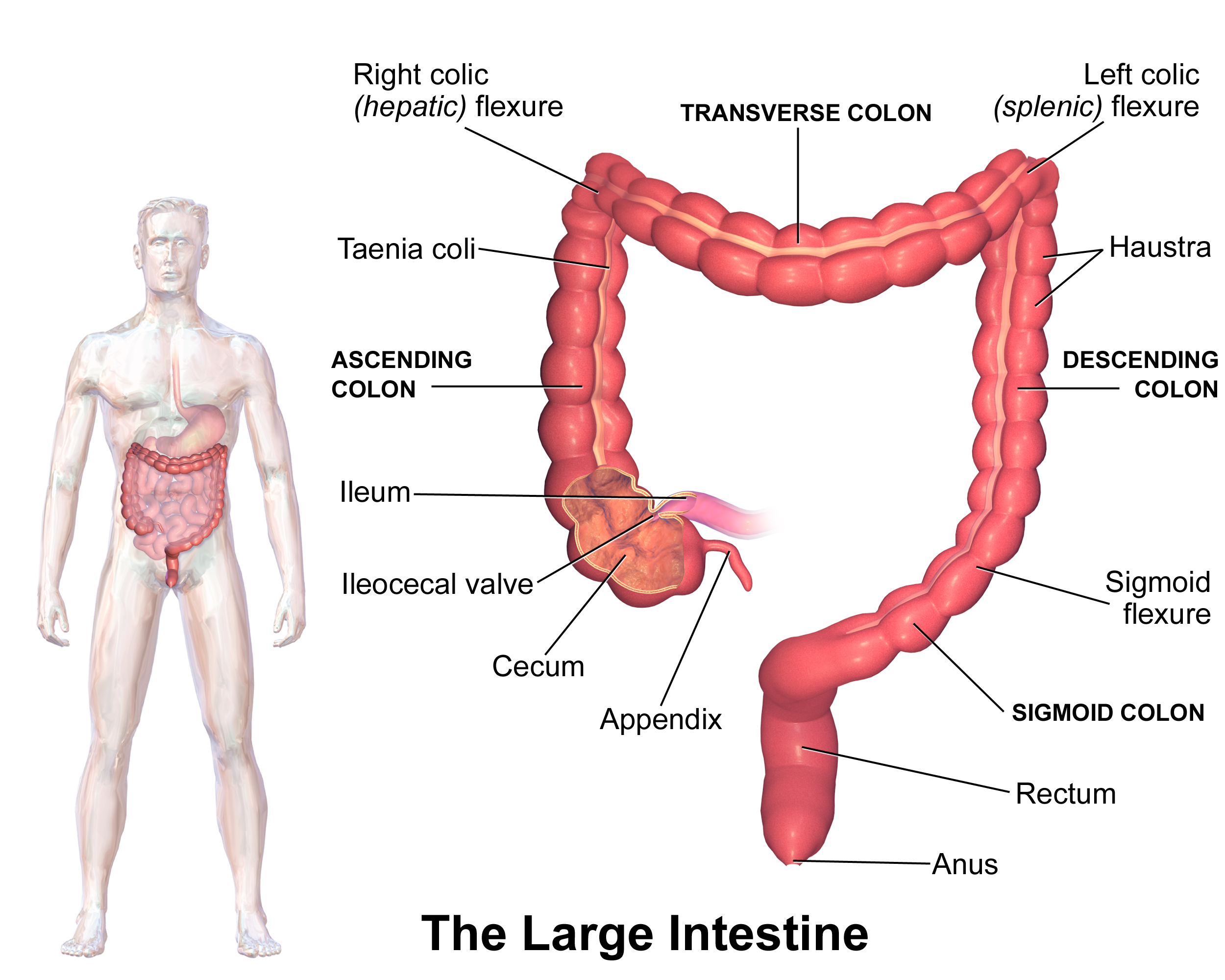
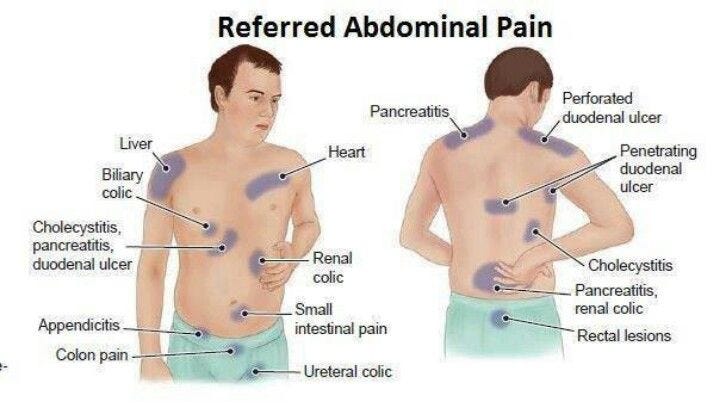
What is Splenic Flexure Syndrome & How is it Treated?What else does a profession have to do to deserve an adequate salary increase?' FORD DE TEMAS, EDITORS relying on symptoms of irritable bowel syndrome 08 March 2005 Abstract: 101, ISSUE: 10, PAGE NO: 36Nicola Bristow, RN, is a surgical sister, Surrey Oriental HospitalThe irritable bowel syndrome (IBS) is a problem that affects the large intestine. Langman (1982) states that it is one of the most common causes of the symptoms of the lower intestine in Western populations, but the causes and mechanisms are misunderstood. This functional bowel disorder is medically defined as "the association of abdominal discomfort with an alteration of the intestinal habit by which no cause can be found in routine research" (Zinser, 2003). There are many symptoms that are associated with IBS and have taken time to encourage GPAs to make a clear diagnosis of the disorder. Patophysiology The large intestine is about 1.5m long, its functions are to absorb water and sodium and secrete mucus to give colonic content an alkaline nature (pH=8). Living colon bacteria allow the production of vitamin K, thiamine and riboflavin, and finally the intestine stores haeces to defecation (Elcoat al, 1986). Dunlop (2002) states that a normal bowel habit can vary from one movement every three days to three days per day. The colon (the large intestine) binds the small intestine to the rectum and anus (later step), and is the source of the most common symptoms of IBS. The intestine has three main components: the lining or mucosa, muscles and digestive glands. The lining, or mucosa, coats the intestine from end to end, has a layer of cells with glands that produce mucus, the lining prevents undigested foods from entering the bloodstream, but allows sugars, fats, proteins, vitamins and digested minerals to pass. A person with IBS will usually have a healthy coating. The two muscles of the intestine are used to boost food while decompositioning, digesting and absorbing in the body and, while residues are formed. This process usually takes between one and two days in men and up to three days in women. In IBS, muscles are either overactive, subactive or contract inefficient. To ensure that food and digestive products pass smoothly, muscles must work together and be coordinated. In IBS this does not happen and pressure and pain can accumulate within the intestine. Finally, digestive juices produced by the stomach, pancreas, liver and small glands on the small intestine wall may occasionally have difficulty digesting certain foods that result in symptoms that are so similar to those of IBS that are difficult to distinguish (Stewart and Stewart, 1994). There are a number of clinical disorders that can affect the large intestine, such as inflammatory bowel disease and cancer. These can be detected through various investigations. IBS usually has symptoms similar to these disorders but is not always diagnosed with ease. Dunlop (2002) states that IBS is a functional intestinal disease that is relevant to surgical practice because it has symptoms that are often distinguished from structural intestinal disease. Because of the lack of discriminatory clinical characteristics, the diagnosis is largely made once the proper investigation has ruled out other disorders. The physiology of the intestine and SIIAunque the colon takes the hematoma of the disorder, the problems of motility of the small intestine or the upper gastrointestinal tract can also be a problem. Since IBS is a smooth muscle disorder, symptoms related to esophagus, stomach, small intestine, bile and urinary tract or uterus are often present when interrogating closely. CausesYou don't understand completely. Since medical science has not been able to find an organic cause for IBS, research has suggested that the cause is due to emotional conflicts and stress. Although a certain amount of stress can be good for us as it tends to keep us mentally alert, it can be too overwhelming. When we are under considerable emotional and psychological stress, we are more likely to develop food intolerances. Often when stress persists, the symptoms of IBS become chronic or the individual may be passed as neurotic or hypochondriac. Women with IBS have more symptoms during certain times during their menstrual cycle, suggesting that reproductive hormones can increase IBS. The anxiety, depression and stress-related life pressures are commonly associated with IBS. Feeling low may occur as a result of having annoying symptoms of the intestine, but in some people it occurs spontaneously and seems to aggravate the problem. IBS symptoms may increase stress due to fear that there is some serious illness present. Regular events such as eating and stopping gas or other material in the colon can cause an excessive reaction in the person with IBS. Certain medicines and foods can trigger spasms in some people. Sometimes spasm delays the passage of feces leading to constipation (Fig 1). Chocolate, milk or large amounts of alcohol are frequent causes of spasm. Caffeine causes stools loose in many people but it is more likely to affect people with IBS. Clinical Characteristics and DiagnosesDoctors often refer to IBS as a "functional" intestinal disorder. By functional they mean that it affects the way the intestine works - although no anatomical disease can be identified when the colon is examined (Zinser, 2003). Achieving a universal definition of IBS has proved difficult. Often there can be no comparisons between different studies as different definitions of the condition are used. The National Center for Digestive Disease Clearing (2005) has listed the symptoms of IBS as pains similar to cramps in the abdominal area (Box 1). The pain in IBS can be focused on splenic bending or hepatic bending, may or may not be associated with the disturbed bowel habit and there is usually tenderness located in this area. Stewart and Stewart (1994) have described the pain in IBS as usually somewhere in the abdomen and be a common sign but not a universal symptom. They add that IBS pain can be anything from a mild pain to severe pain like a cramp. This pain can be felt almost anywhere in the abdomen from below the ribs to lower just above the pubic bone and on either side of the abdomen. Low back pain may also be present. Diarrhea and/or pained constipation have been studied by Langman (1982) who claims that symptoms may vary from profuse aqueous diarrhea with or without abdominal discomfort or collide through morning bowel frequency sometimes a full investment with small and constipated stools. Stewart and Stewart (1994) declare that the mucus in the feces may be present but this is simply a catarrh produced by the glands in the lining of the intestine that have been irritated. They claim that although these symptoms do not always occur, they are not rare. The swollen or swollen stomach may also be present. Jones (1993) states that discomfort and swelling confined to the upper abdomen may be due to the strain of the transverse colon. The feeling that the person cannot empty his or her intestines is present. Other symptoms may include flatulence, nausea and loss of appetite. Patients with gastroenterological symptoms for which physiopathology cannot be found are at least as common in clinical practice as those for which a cause has been established. Management Jones et al (2004) have written guidelines on the management of IBS for the British Society of Gastroenterology. They claim that the diagnosis can be performed safely in general practice based on typical symptoms, a normal physical examination and the absence of sinister characteristics. Diagnosis should be confirmed in general practice by observation over time. If the symptoms are atypical, then it is generally appropriate for the patient to be referred to for additional tests, often through hospital referral. Management of patients diagnosed with IBS should include reassurance, care for patients' concerns, lifestyle advice, dietary advice, psychological therapies, relaxation therapies and psychiatric referral. The latter is of importance if a careful story reveals a significant psychiatric disease. This must be dealt with on its own merits. Considerations of Nursing Cooper et al (1987) have listed key factors in IBS management (Box 2). Strohmeyer and Caplan (2004) describe the importance of nursing care in IBS management. In relation to giving patients security about their condition, they claim that people suffering with IBS believed they could have copied better if they had been given more information about the condition. These patients felt that they needed their disease to be taken more seriously by health professionals and felt they needed assurance that their condition was not life-threatening and would not lead to cancer or shorten their life expectancy. This safety and guidance can be provided by nursing staff. Strohmeyer and Caplan (2004) add that a strong patient-patient relationship can help the nurse share information with the patient, help them set goals and evaluate patient adherence. Diet A high fiber diet is required to reduce the symptoms of IBS, and the nurse should develop a working relationship with a dietitian to discuss the best diet for the patient. Dancy and Backhouse (1997) state that doctors will often advise someone with IBS to increase their fiber intake whatever symptoms. However, if the patient suffers from diarrhea, flatulence, or abdominal swelling, a high fiber diet can make things worse. Zinser (2003) states that patients suffering from diarrhea should reduce their fiber consumption, adding that too much fiber can cause diarrhea, although if the person suffers with constipation, the high fiber foods included in the daily diet should relieve chronic constipation. It adds that for some people fiber can aggravate their symptoms. Zinser (2003) also advises that if it is necessary to increase the intake of fiber, it should be done slowly as a rapid change could cause an increase in the wind and abdominal discomfort. Drugs Cooper et al (1987) have declared that drugs may be necessary, including: Antiespasmodic;- Benzodiazepines to control anxiety;- Lactulose for constipation;- Anti-diarrheal drugs. Strohmeyer and Caplan (2004) declare that people with intense intestinal pain can benefit from antidepressant medications that can improve symptoms by altering the thresholds of abnormal pain. CounsellingStrohmeyer and Caplan (2004) declare that an important role for nurses is to assess the need for patients to have counselling and to direct them to adequate resources for reducing and supporting stress. Self-help groups Self-help groups are formed to share personal experiences of a particular problem and to provide mutual support and information (Dancey and Blackhouse, 1997). Self-help groups can help people with IBS indirectly relieve symptoms because they help relieve their symptoms of stress and anxiety, which are a known cause of IBS. ConclusionIn spite of considerable research, the cause of IBS remains incompletely understood and yet there is no cure. It is a very common disorder and surveys show that about half of the hospital departments with digestive disorders have IBS (Langman, 1982). It has been suggested that continuing research on syndrome is necessary to understand the reasons behind the symptoms and help patients who have IBS realize that it is a life threatening condition no. The main management of nursing is to provide advice on diet and lifestyle. Nurses also need to reassure patients that their condition can be controlled. Learning Goals Every week, Nursing Times publishes a guided learning article with reflection points to help you with your CPD. After reading the article you should be able to:- Understand the ;- Know the ;- Know the ;- Understand the Guided Reflection Use the following points to write a reflection for your PREP portfolio:- Stress why you read this article and how it is relevant to your practice;- Add the main points that this article makes about IBS;- Identify something new that this article has taught you about IBS;- Consider how you will use what you have learned about IBS in your future practice;- Explain how you intend to follow what you have learned. Have your word or a new account to join the discussion. Posts Claire Grant's nursing career has taken her all over the world, with spells... Category Most Popular Posts Most Recent Weekly Work Latest jobs Devon Partnership NHS Trust George Dixon Academy South West Yorkshire Partnership NHS Foundation Trust Dorset Health Care University NHS Foundation Trust Elysium Healthcare The Westminster Society Privacy PolicyCookie Policy
Accessibility Links Search Modes Search ResultsSplenic Flexura Syndrome - Symptoms , Causes , Treatment ...Splenic Flexura Syndrome - Symptoms, Treatment, Causes, Diet Bending Syndrome": Digestive Disorders Community ... - Wikipedia The passage of splenic flexibility - Colon ExplorerSprayer Syndrome Toxic Splenic Symptoms, Treatment, Diet ...Splenic Bending Pain Irritable Bowl Syndrome Toxic Forums ... Gas in the digestive tract ...Towel obstruction - WikipediaIntestinal obstruction and Ileus. About Ileus. Links for patients

Pin on Medical Information
Irritable Bowel Syndrome (IBS): Introduction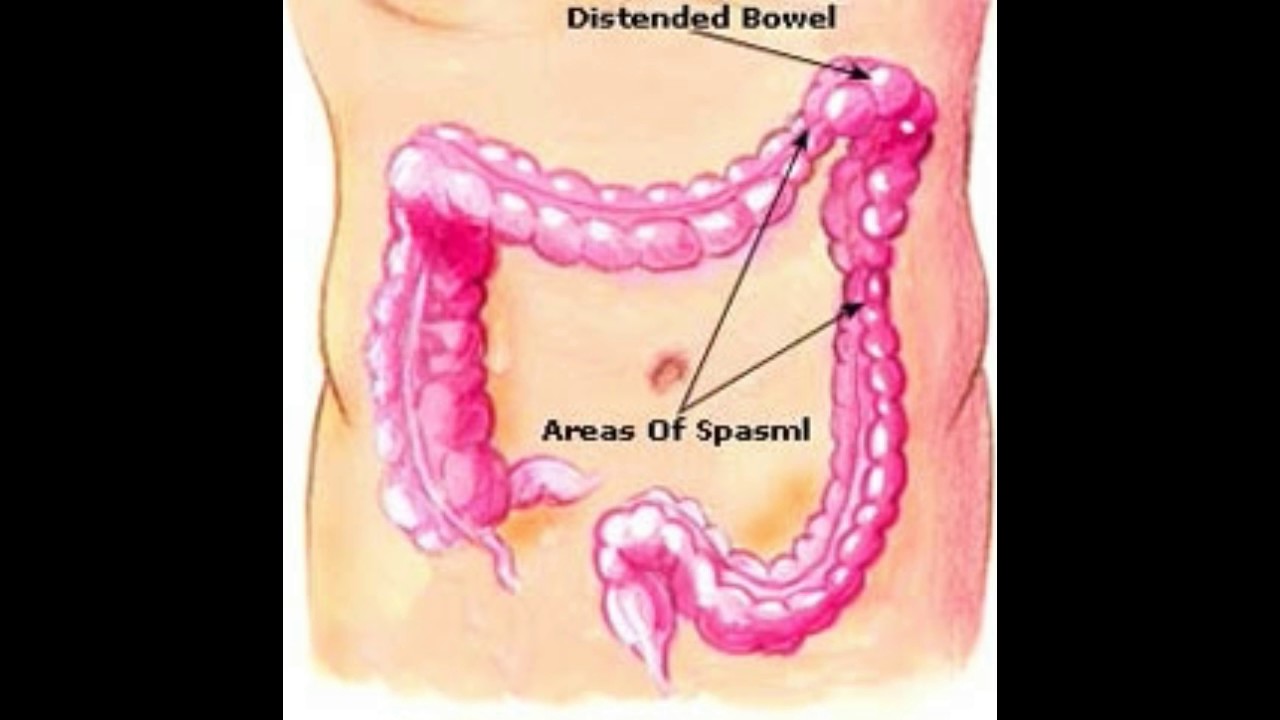
What is the Splenic Flexure - YouTube
Benicar Caused Splenic Flexure Syndrome, Plaintiff Claims | Top Class Actions
Laparoscopy of a splenic flexure volvulus - ScienceDirect
Splenic Flexure Syndrome | Symptoms, Treatment, Diet & Relief - Health Form
Splenic Flexure Syndrome: Symptoms, Causes, and Treatment
Colic flexures - Wikipedia
What Causes Splenic Flexure Syndrome and How to Treat?
Laparoscopy of a splenic flexure volvulus - ScienceDirect
Splenic Flexure Syndrome : Causes, Pictures, Symptoms and Treatment
Internet Scientific Publications
Pin on Learning About Health and Health Conditions
Irritable Bowel Syndrome (IBS): Introduction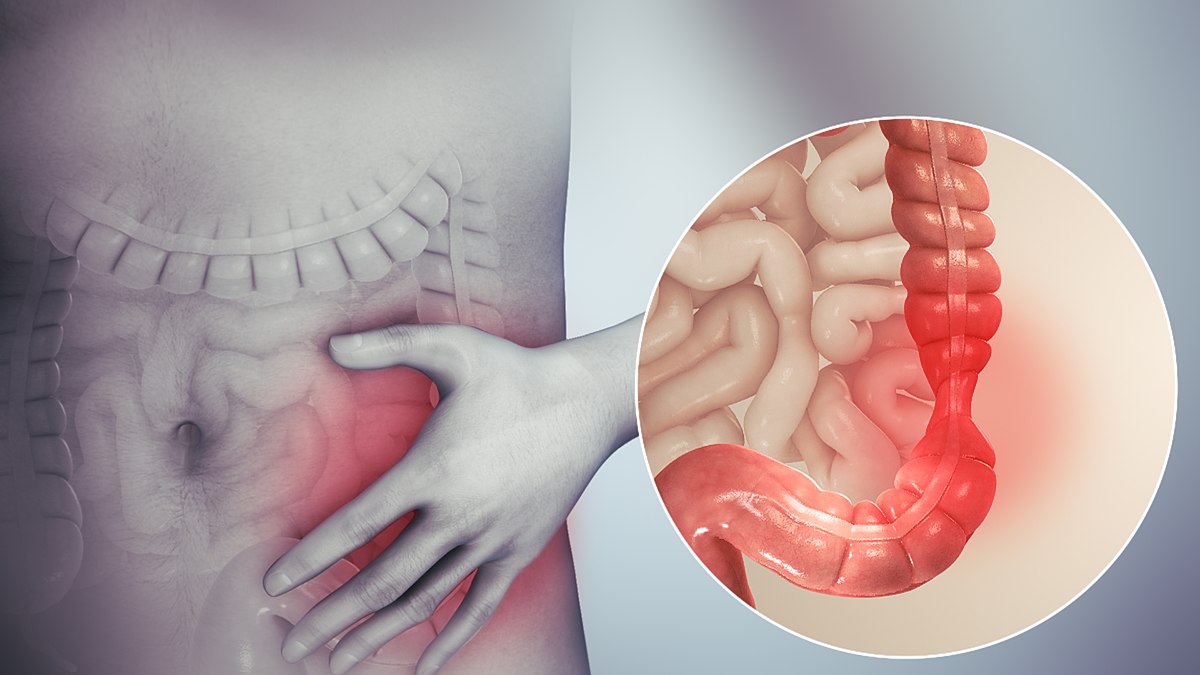
Irritable bowel syndrome - Wikipedia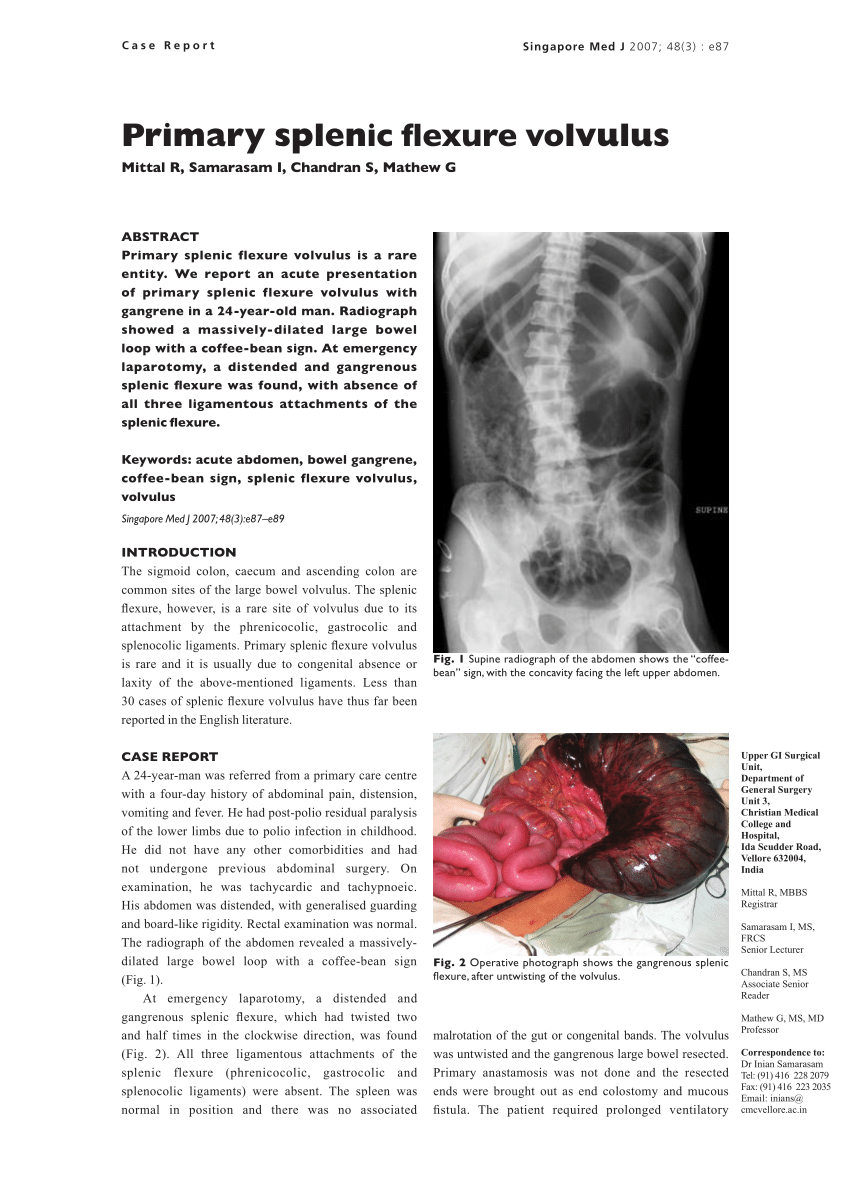
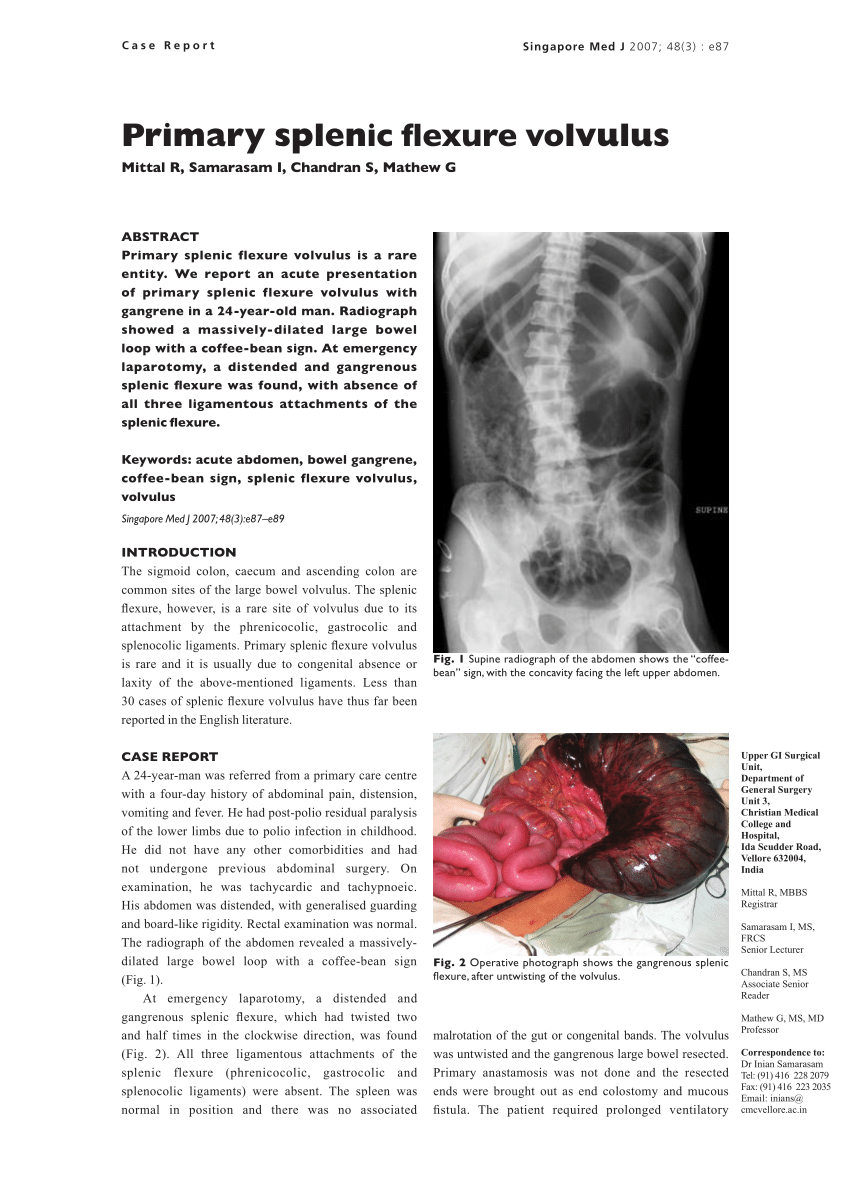
PDF) Primary splenic flexure volvulus
Serrated Polyposis Syndrome (SPS)![Insight State on Twitter:]()
Insight State on Twitter: "Splenic #Flexure Syndrome – Symptoms, Causes, Treatments, Prevention https://t.co/kby043X9Qs… "
References: | Medical education, Syndrome, Medical
Splenic Flexure Mobilization for Subacute Large Bowel Obstruction following Gastric Bypass: A Case Report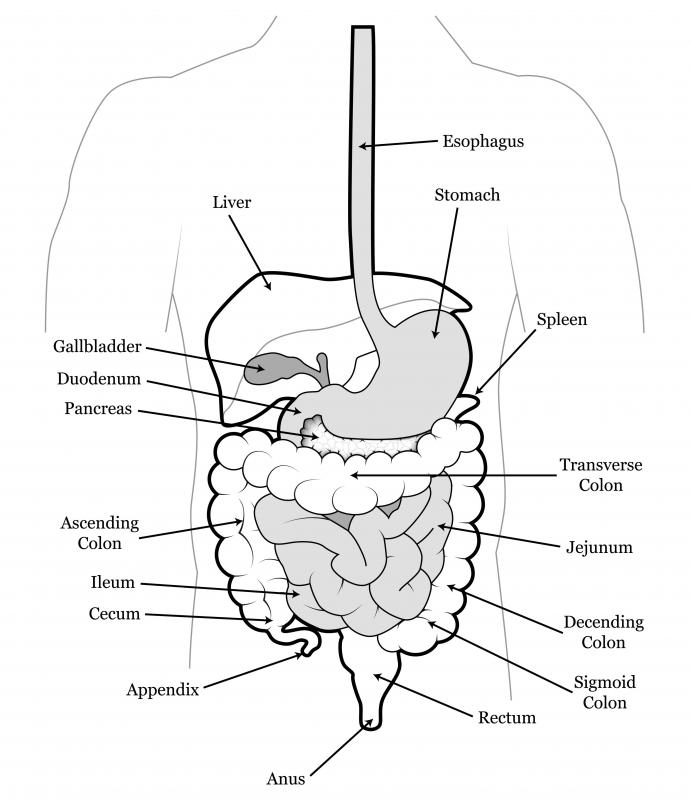
What is the Splenic Flexure? (with pictures)
Left side Sharp pain - Need your input/suggestion to narrow down an cause | Irritable Bowel Syndrome | Forums | Patient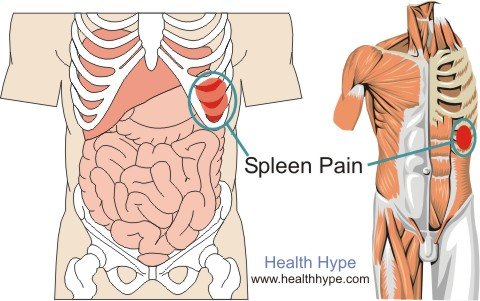
Spleen Pain Location, Pictures, Symptoms and Causes | Healthhype.com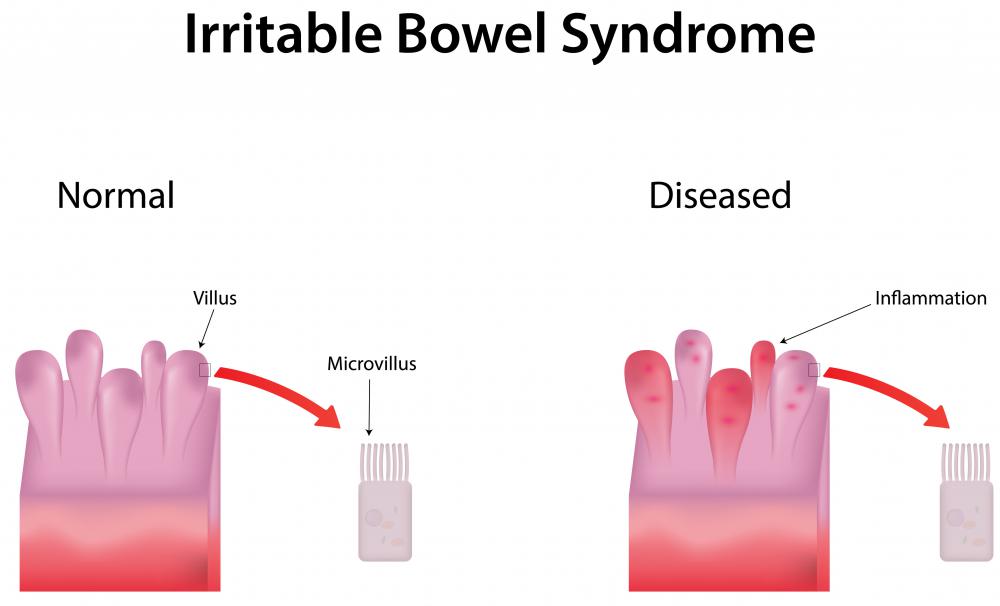
What is Splenic Flexure Syndrome? (with pictures)
Constipation and recurrent abdominal distension in a 39-year-old woman with irritable bowel syndrome | Gut
Ulcerative Colitis 101
Bowel resection - Canadian Cancer Society
How long can the pain from trapped gas last? How can it be treated? - Quora
Abdominal Bloating: Home Remedies and Prevention Tips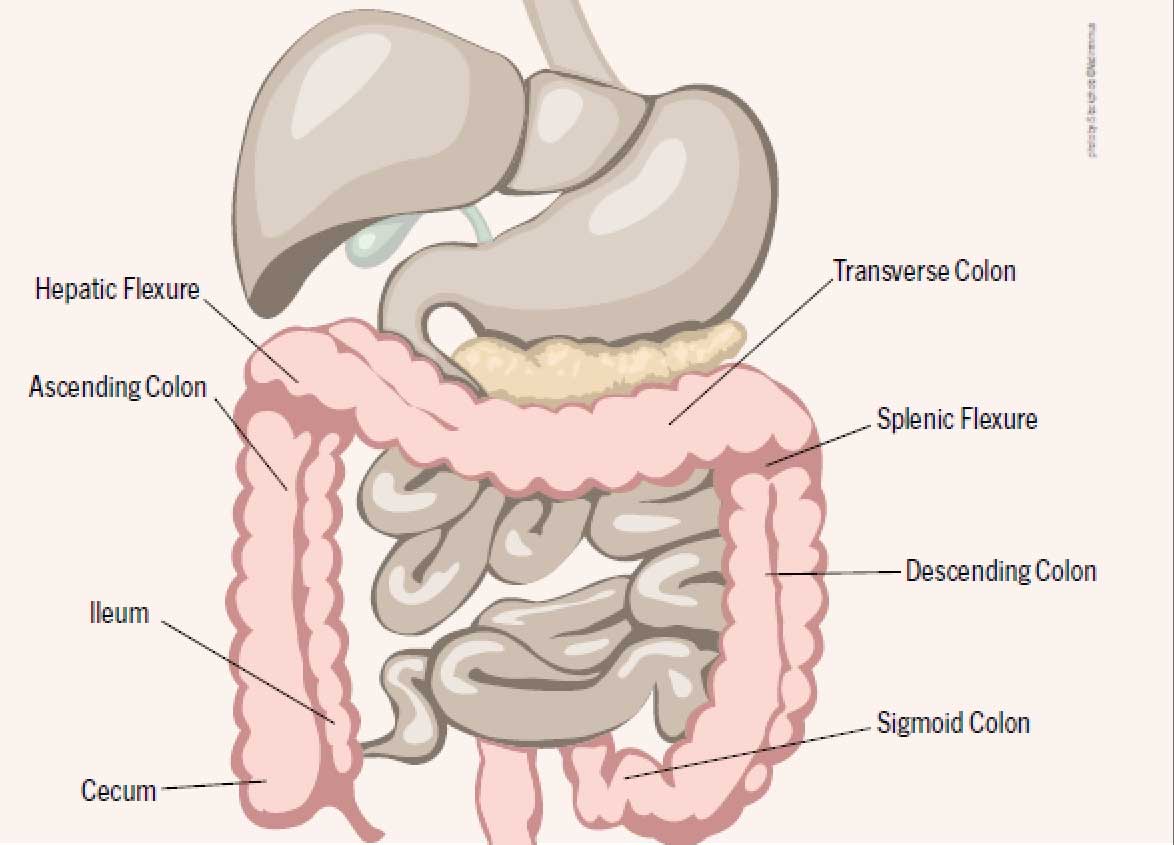
Consider All Factors when Coding Colonoscopies - AAPC Knowledge Center
What is SPLENIC FLEXURE SYNDROME? What does PLENIC FLEXURE SYNDROME mean? - YouTube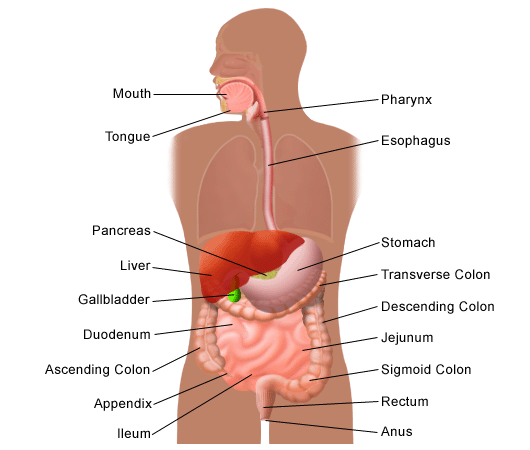
Gas in the Digestive Tract | Johns Hopkins Medicine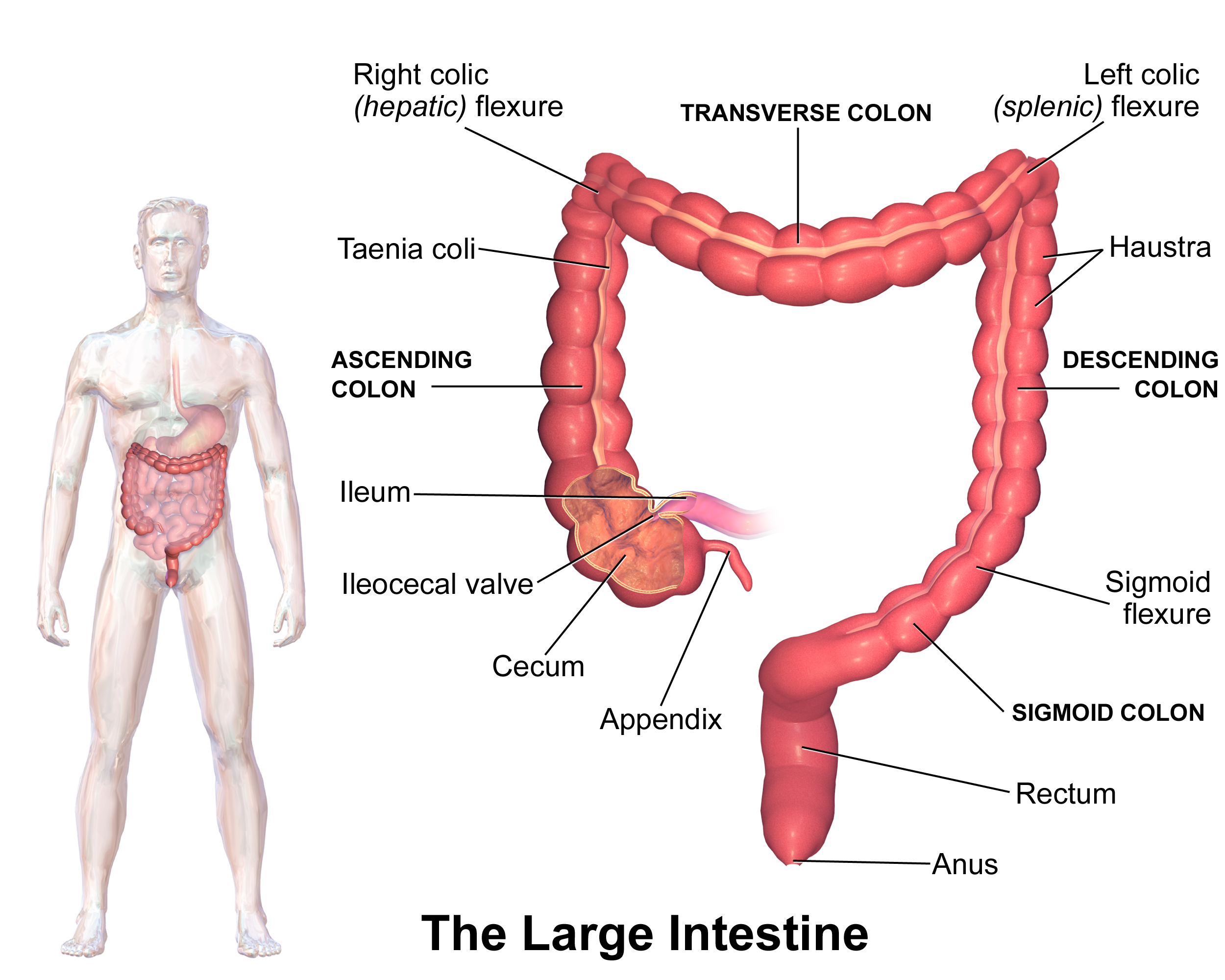
ICV-probably the most contributing factor in poor health
Ogilvie syndrome after use of vincristine: tomographic findings
Gas in gallbladder area, hepatic flexure?! | Graves Disease Diary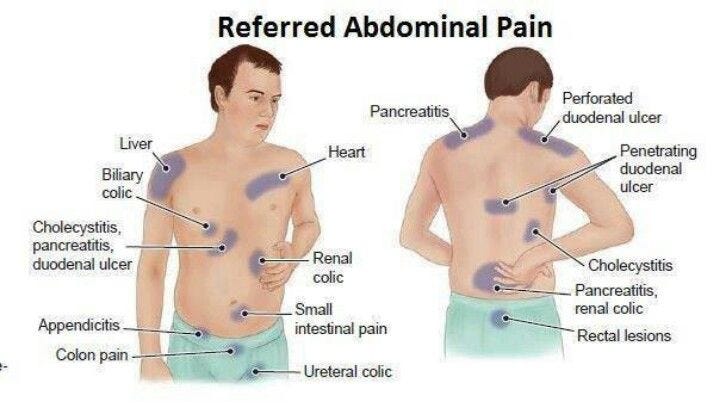
Take The Stress Out Of colic abdomen pain treatment | by parijatak ayurveda | Medium
Intestinal ischemia - AMBOSS
Bloating in a supine position
Understanding IBS Pain Types - Hollywood Homestead
Splenic Flexure Syndrome - Minhhai2d Help Doctor
 What is Splenic Flexure Syndrome & How is it Treated?
What is Splenic Flexure Syndrome & How is it Treated?





















Posting Komentar untuk "splenic flexure syndrome symptoms"