how to treat vulvar ulcers
 Genital ulcers - Clinical guidelines
Genital ulcers - Clinical guidelines10 Causes of Vulvar Ulcers and How to Treat themWe include products that we believe are useful to our readers. If you buy through links on this page, we can win a small commission. What are vulvar ulcers? Vulva is the outer part of a woman's genitals. The Vulvaran ulcers are ulcers that appear in this area. Vulvar ulcers can be extremely painful and, in some cases, they cannot hurt at all. Most of the time these injuries are caused by but many other problems can trigger an ulcer. There are several effective treatment options for these sores. Read more about what causes vulvar ulcers and how to treat them. Vulvar ulcers look like blows or rash. Or, sores like skin breaks that expose the tissue. The symptoms of vulvar ulcers vary, but may include: Sometimes vulvar ulcers do not cause symptoms. Usually, vulvar ulcers are classified as sexually acquired or not sexually. A sexually acquired vulvar ulcer means that the injury is the result of sexual contact. This is the most common type of genital ulcer. Sexually unearthed ulcers are also called acute genital ulcers. These are more common in young women who are not sexually active. There are many possible reasons for developing vulvar ulcers, including:1. STIsThe most common cause of genital ulcers in the United States is the virus (VHS), followed by . Other sexually transmitted infections can lead to ulcers, including: In addition, some women with can develop ulcers in their genitals. Sexually transmitted infections are more common than you might think. According to the , 1 in 2 people who are sexually active will contract an STI at 25 years. Fungal infectionsVulvovaginal candidiasis, also known as , is the most common fungal infection that causes ulcers or vulvar erodes. Other symptoms of yeast infections include:3. Viral InfectionsThe arteries virus can cause vulvar ulcers to form:4. Bacterial infections Bacterial infections, such as A Streptococcus and mycoplasm, can trigger vulvas. Bacterial infections are usually treated with antibiotics.5. Inflammatory diseasesThe types of inflammatory and autoimmune diseases can cause lesions in the form around the vulva. Depending on the severity of these are, they may appear as ulcers. Some of these include:6. TraumaChronic frost or vulva scratch may lead to skin and ulcer irritation.7. Other diseasesSometimes common conditions such as , , or a virus that causes diarrhea can cause genital ulcers, especially in adolescents.8. Drug reactions Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), sulfonamides and certain antibiotics can cause a reaction that triggers ulcers.9. Cancer can cause lesions similar to ulcers around the vagina. This type of cancer is more common in older women. 10. Skin reactionsSometimes, a skin care product can cause a genital ulcer. You might want to change soaps and lotions for sensitive skin if this happens. Around the world, people develop some kind of genital ulcer disease every year. Types 1 and 2 of HSV are the most common causes of genital ulcers in the United States. and 14 to 49 years old has VH 2 genital infection. Your doctor will probably perform a physical exam and explore your health history to determine what is causing your vulvar ulcers. You might be asked about your sexual life, number of sexual partners, and what medications you take. Also, your doctor will have to look at the ulcer or ulcers to get a better idea of what might be causing. Your doctor may recommend one or more of the following tests: You may also need a biopsy. A biopsy is a procedure that involves removing a sample from the ulcer and sending to a laboratory for further examination. Your treatment approach will depend on what your ulcers are causing. Some vulvar ulcers may disappear on their own, but others require quick therapy so they don't lead to infection. Your doctor may recommend several types of therapies to treat your condition. Sexually transmitted infections are typically treated with antibiotic and antiviral medications, given as a pill or an injection. Vulvar ulcers that are not caused by infections can be treated with: Your healthcare provider may show you how to effectively clean your ulcer until it is cured. You may also need special dressings to cover and protect the area. Sometimes home remedies can be used to relieve pain and discomfort of vulvar ulcers. Popular methods include: Shop for , , , and . If vulvar ulcers are untreated, they can cause complications. In some cases, scarring, adhesions, infection and inflammation may occur in or around your genitals. In addition, untreated ulcers can lead to ongoing pain and emotional stress. If you have an untreated STI, you are at risk of getting another one. You can also spread the infection to others. Some sexually transmitted infections can cause serious problems. For example, the nervous system without treating syphilis and heart problems. And if you become pregnant, a STD can affect the fetus. Many sexually transmitted infections can be cured or given with proper treatment. Other causes of ulcers can be helped with the right therapies. You may be able to prevent or reduce the risk of a vulvar ulcer by practicing safe sex and be tested for sexually transmitted infections regularly. If your vulvar ulcer is caused by another medical condition, such as an inflammatory or autoimmune disease, it may be referred to a specialist who can help treat your condition. Although vulvar ulcers may cause shame, you should see your doctor immediately if you develop them. You don't have to live with the pain, discomfort and anguish that these injuries commonly cause. Last medical review on May 3, 2018
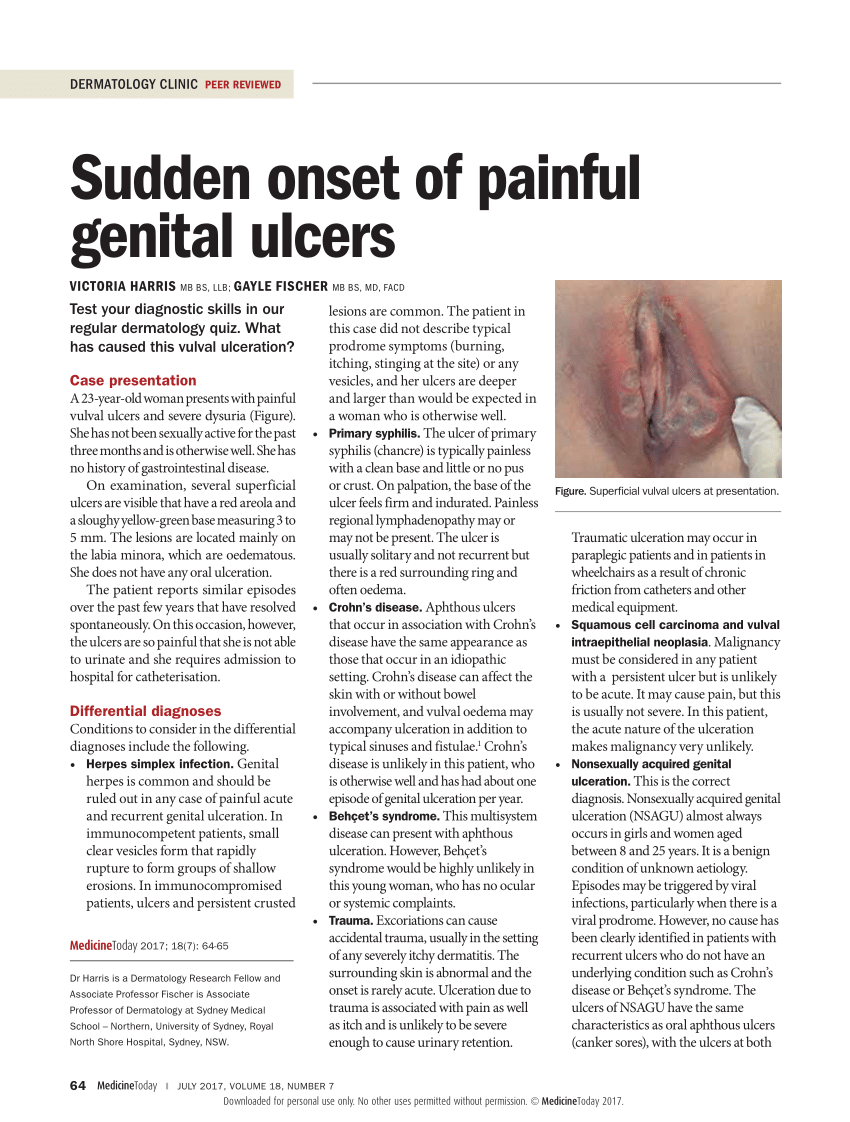
PDF) Sudden onset of painful genital ulcers

Superficial Ulceration on the Vulva | MDedge Dermatology

Vulval ulcer images | DermNet NZ
Genital ulcer
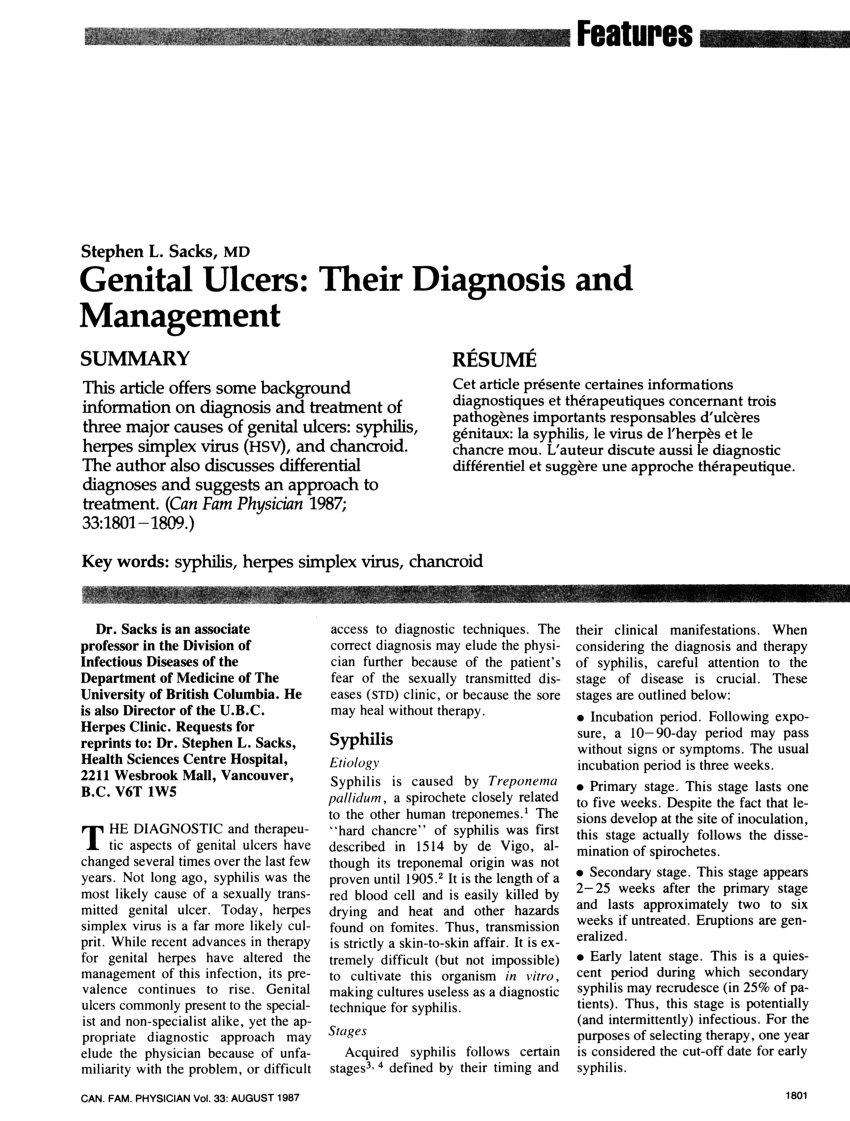
PDF) Diagnosis and Management of Genital Ulcers

Genital ulcers: do not forget Behçet disease | BMJ Case Reports

Chancroid and human immunodeficiency virus infection – a review - Mohammed - 2008 - International Journal of Dermatology - Wiley Online Library

Vulval ulcer images | DermNet NZ
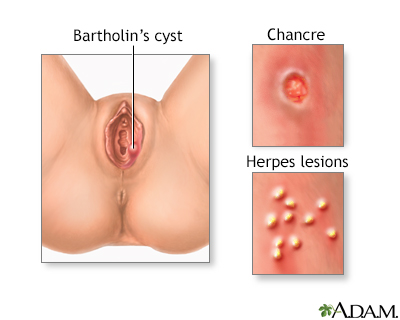
Genital sores - female Information | Mount Sinai - New York

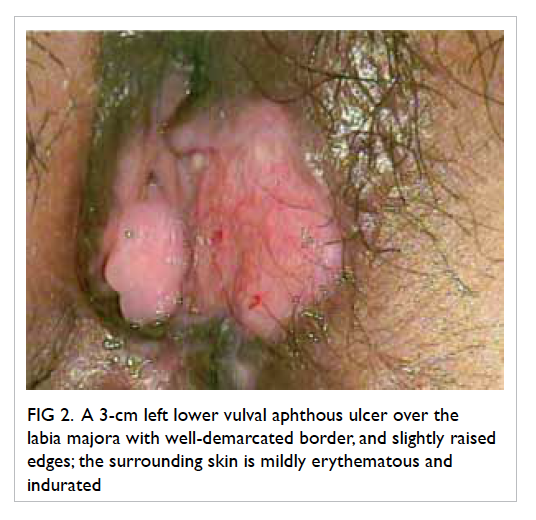
Vulvar Aphthous Ulcer | Consultant360
HIV Genital Sores Singapore | HIV Genital Sores | Shim Clinic
Lipschütz ulcer (ulcus vulvae acutum): a rare cause of genital lesion

Successful treatment of genital ulcers with infliximab in Behçet's disease | Annals of the Rheumatic Diseases

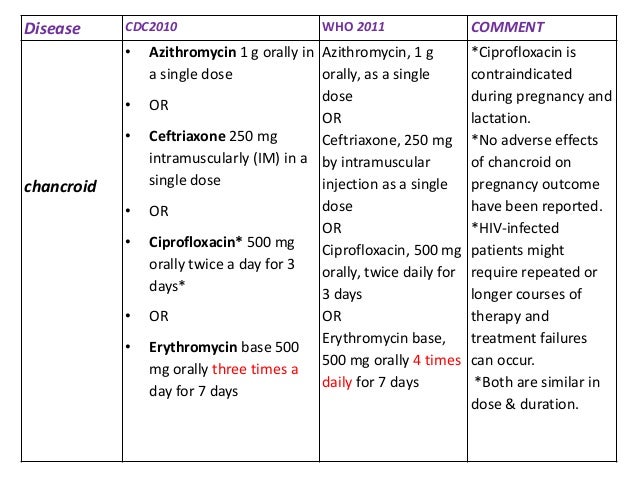
Chancroid - Vulvar Ulcers Treatment - Ulcer Choices

Benign Disorders of the Vulva and Vagina - Current Diagnosis & Treatment Obstetrics & Gynecology, 11th Ed.

PDF) Tuberculosis at vulva and vagina
![PDF] Diagnosis and management of genital ulcers. | Semantic Scholar PDF] Diagnosis and management of genital ulcers. | Semantic Scholar](https://d3i71xaburhd42.cloudfront.net/7258b38456d9447247474406011acc76d516f6e9/1-Table1-1.png)
PDF] Diagnosis and management of genital ulcers. | Semantic Scholar
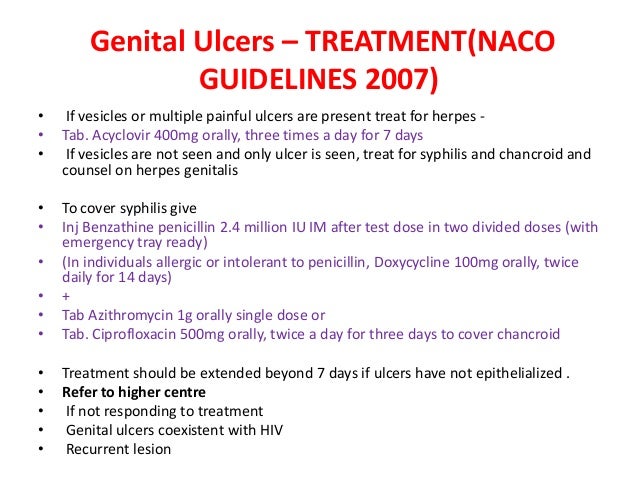
Guidelines for the Management of Sexually Transmitted Infections: 2. TREATMENT OF STI-ASSOCIATED SYNDROMES: 2.2. Genital ulcer: Genital ulcer and HIV infection

Genital ulcer

A persistent vulval ulcer | The BMJ

Ulcers Vulva: Symptoms, Causes, Diagnosis, Treatment, and More
Use of colposcopy in a patient with recurrent genital ulcers | HKMJ

Female Genital Ulcer - NeoHealth ︳創健醫療

Diagnosis of Genital ulcers – How to Remember: MD/MS Entrance Preparation

Vulvar ulcers: Causes, symptoms, and treatments

Epidemiology of Haemophilus ducreyi Infections - Volume 22, Number 1—January 2016 - Emerging Infectious Disease journal - CDC
Top 8 Home Remedies on Twitter: "Genital ulcers come from STI's. The only way to prevent them is through safe sex. Learn more about them with our newest article! https://t.co/csUBoYzVWD #genitalulcer #STI #

Vulvar Aphthous Ulcer | Consultant360

Chancroid - Chancroid Cure
Gale Academic OneFile - Document - Lipschutz Genital Ulceration as Initial Manifestation of Primary Sjogren's Syndrome
Genital ulcer

PDF) Diagnosis and Management of Genital Ulcers
/herpes-treatment-3133020_color1-5b85557ac9e77c00576df991.png)
Effective Treatments for Herpes

Genital ulcer severity score and genital health quality of life in Behçet's disease – topic of research paper in Clinical medicine. Download scholarly article PDF and read for free on CyberLeninka open
The Treatment of Chronic Recurrent Oral Aphthous Ulcers (03.10.2014)
Lipschütz's acute vulvar ulcer: a systematic review | SpringerLink

COVID‐19‐related acute genital ulcers - Falkenhain‐López - 2020 - Journal of the European Academy of Dermatology and Venereology - Wiley Online Library

Sexually Transmitted Diseases - Obstetrics and Gynecology 7 Ed.

Vulvar Ulcers | Plastic Surgery Key

Table 3 from Diagnosis and management of genital ulcers. | Semantic Scholar
Posting Komentar untuk "how to treat vulvar ulcers"